There are a lot of medical conditions out there that are pretty clear-cut. They have a single cause, predictable symptoms, and direct, effective treatments. If you’re dealing with something like this, getting a diagnosis and finding relief is simple.
However, there are other conditions out there, like polycystic ovarian syndrome (PCOS), that are a lot more complex. In reality, they make every part of the process, from diagnostics to treatment, really complicated.
Because PCOS is multifaceted and presents a wide range of symptoms, it’s often mistaken for other conditions. Getting the wrong diagnosis can be a big deal—you’re unlikely to find a good treatment plan if the root cause isn’t identified correctly. Therefore, it’s useful to look at other conditions that can look or feel like PCOS. That way, you can be certain you’re taking the right action to reverse your condition and live symptom-free.
Here are conditions with symptoms that overlap with PCOS:
What Can Be Mistaken for PCOS: Conditions with Similar Symptoms
The reason so many conditions get mistaken for PCOS is simple: polycystic ovary syndrome affects so many body functions that it creates a long list of symptoms. Naturally, other conditions can have overlapping signs, which leads to confusion.
I’m going to walk you through several conditions commonly confused with PCOS so you can feel confident about your diagnosis. But first, it’s helpful to know the key symptoms of PCOS. With this list, you can hopefully spot the distinct signs of other conditions that may point to a different underlying issue.
Common Symptoms of Polycystic Ovary Syndrome (PCOS) include:
- Irregular periods
- Absent periods
- Heavy menstrual bleeding
- Infertility
- Difficulty ovulating
- Pelvic pain
- Enlarged ovaries or polycystic ovaries
- Low libido
- Acne
- Darkened skin patches
- Oily skin
- Skin tags
- Excess facial hair
- Excess body hair
- Scalp hair thinning
- Nail brittleness
- Weight gain
- Sugar cravings
- Bloating
- Swelling or water retention
- Mood changes
- Fatigue
- Headaches
Hormonal/Endocrine Disorders
Though we’re not sure what triggers PCOS, there’s always a hormonal component. Usually, women with PCOS have imbalances of stress, thyroid, and reproductive hormones. In turn, this causes symptoms like irregular periods, excess hair growth on the face and body, weight gain, infertility, and mood problems. (Just to name a few.)
Hypothyroidism
Hypothyroidism occurs when your thyroid gland is underactive. That means it doesn’t make enough thyroid hormones (T3 and T4) to regulate your metabolism, energy levels, body temperature, and other essential functions.
It can be mistaken for PCOS because thyroid hormones are often out of balance in both conditions. The key difference is that PCOS involves imbalances in multiple hormones, not just thyroid levels.
So, if your thyroid symptoms are the most prominent, you may receive a hypothyroidism diagnosis before your condition is recognized as PCOS. But even after correcting thyroid hormone levels, other imbalances (like high androgens, elevated cortisol, and low progesterone) still need to be addressed.
Here’s more on PCOS and hypothyroidism.
Overlapping Symptoms of PCOS and Hypothyroidism:
- Irregular menstrual cycles
- Infertility
- Weight gain or difficulty losing weight
- Fatigue
- Depression or mood swings
- Brain fog
- Thinning hair or hair loss
- Dry skin
- Acne
Distinct Symptoms of Hypothyroidism:
- Feeling unusually cold
- Constipation
- Hoarseness/deep voice
- Carpal tunnel syndrome
- Slow heart rate
Hyperprolactinemia
Hyperprolactinemia occurs when your body’s prolactin levels are too high. This is the hormone that helps with milk production after pregnancy. However, a pituitary gland tumor, thyroid issues, high stress, or even certain medications can elevate prolactin levels. This can happen even if you’re not nursing.
Since PCOS affects the reproductive system, some symptoms can overlap, leading to a misdiagnosis. However, women with PCOS rarely have high prolactin levels. Their reproductive symptoms are instead due to high testosterone, low progesterone, and high estrogen. So, if you’re experiencing excessive milk production, you’re probably not dealing with PCOS. It’s more likely hyperprolactinemia.
Overlapping Symptoms of PCOS and Hyperprolactinemia:
- Irregular or absent periods
- Infertility
- Low libido
- Vaginal dryness
- Breast tenderness
- Fatigue
- Depression and mood swings
Distinct Symptoms of Hyperprolactinemia:
- Galactorrhea (milk production when not pregnant or breastfeeding)
- Vision changes
Cushing’s Syndrome
Cushing’s syndrome occurs when your body has unusually high cortisol (stress hormone) levels over a long period. Certain medications that can trigger this, but it can also come from tumors on the adrenal or pituitary gland.
It’s sometimes mistaken for PCOS because Cysters also have elevated cortisol levels. However, PCOS has other hormonal imbalances besides high cortisol levels. So, some symptoms will be overlapping, but you’ll likely have a longer list of symptoms with PCOS than you would with Cushing’s Syndrome.
Overlapping Symptoms of PCOS and Cushing’s Syndrome:
- Irregular or absent periods
- Infertility
- Weight gain
- Excess facial or body hair
- Acne
- Depression and mood swings
- Fatigue
Distinct Symptoms of Cushing’s Syndrome:
- Thin arms and legs
- Purple stretch marks on the abdomen, thighs, or breasts
- Easy bruising
- Muscle weakness
- Slow wound healing
- Increased susceptibility to infections
Congenital Adrenal Hyperplasia (CAH)
Congenital Adrenal Hyperplasia (CAH) is a genetic disorder that affects the adrenal glands, leading to elevated androgen levels. Because PCOS involves high androgens, it’s easy to understand how the two conditions can become mixed up. However, since CAH is genetic, the symptoms show up at birth or early childhood. In contrast, PCOS doesn’t set in until puberty or early adulthood.
Overlapping Symptoms of PCOS and Congenital Adrenal Hyperplasia:
- Irregular or absent periods
- Infertility
- Excess facial or body hair
- Acne
- Scalp hair thinning
- Weight gain
Distinct Symptoms of Congenital Adrenal Hyperplasia:
- Early signs of androgen excess in childhood (ambiguous genitalia or early pubic/axillary hair)
- Severe body odor
- Rapid growth in childhood but short adult stature (due to early bone maturation)
- Salt-wasting
Androgen-Secreting Tumors
These are rare, but sometimes tumors on the ovaries or adrenal glands can produce excess androgens. Since PCOS also involves high levels of androgens, these conditions can be confused. That said, PCOS hormonal imbalances are more gradual and chronic, whereas androgen-secreting tumors will suddenly spike those male hormones. So, if your symptoms are totally new and come about rapidly, it could be an androgen-secreting tumor rather than PCOS.
Overlapping Symptoms of PCOS and Androgen-Secreting Tumors:
- Irregular or absent periods
- Infertility
- Hirsutism
- Acne
- Scalp hair thinning
- Weight gain
Distinct Symptoms of Androgen-Secreting Tumors:
- Rapid onset of severe hirsutism
- Sudden male-pattern baldness
- Deepened voice
- Clitoral enlargement (virilization)
- Extremely high androgen levels in blood tests
Reproductive System Conditions
A sex hormone imbalance is a core feature of PCOS and often drives its symptoms. That means many side effects of PCOS impact reproduction and menstruation. So, it’s not surprising to hear that polycystic ovary syndrome is sometimes mistaken for reproductive conditions that have similar symptoms (though different root issues).
Endometriosis
Endometriosis occurs when uterine tissue grows outside the uterus, often on the ovaries, fallopian tubes, or pelvic lining. This can result from factors like retrograde menstruation or immune system dysfunction, but the condition is primarily a physical problem. All symptoms of endometriosis stem from excess tissue in the wrong places.
As you can imagine, endometriosis can be quite painful and may cause reproductive issues. Because women with PCOS also experience menstrual irregularities and reproductive symptoms—and sometimes pelvic discomfort or even ovarian cysts—endometriosis can be confused for PCOS.
However, PCOS is a hormonal condition, and hormonal imbalances usually cause its symptoms, not physical tissue growth like in endometriosis. In cases of endometriosis, doctors usually won’t find significant hormonal imbalances. Instead, diagnosis often relies on a laparoscopy, a pelvic exam, or imaging tests to reveal the excess tissue.
Here’s more on PCOS and endometriosis.
Overlapping Symptoms of PCOS and Endometriosis:
- Irregular or absent periods
- Severe menstrual cramps (less severe with PCOS)
- Infertility
- Fatigue
- Pelvic discomfort
Distinct Symptoms of Endometriosis:
- Severe menstrual cramps
- Pain during sex
- Severe pelvic pain
- Pain with bowel movements or urination
- Scarring or adhesions
Uterine Fibroids
Polycystic ovary syndrome isn’t really named accurately—“polycystic ovaries” are just one symptom, and not every Cyster will have them. That said, ovarian cysts can be super annoying for some people. If pelvic pain, discomfort during sex, or bloating from cysts are your main symptoms, it can sometimes be mistaken for endometriosis or uterine fibroids.
Uterine fibroids are noncancerous growths within the uterine muscle, whereas ovarian cysts are fluid-filled sacs on the ovaries. The symptoms can be similar, but few women with PCOS experience only ovarian cysts. Usually, there’s a long list of other chronic symptoms. So if you have additional signs of hormonal imbalance beyond cysts, you’re more likely to have PCOS.
Overlapping Symptoms of PCOS and Uterine Fibroids:
- Irregular or heavy periods
- Infertility
- Pelvic discomfort or bloating
- Fatigue
Distinct Symptoms of Uterine Fibroids:
- Pelvic pressure or a sense of fullness
- Enlarged uterus/visible abdominal bulge
- Frequent urination or urinary urgency
- Constipation or rectal pressure
- Pain during sex
Premature Ovarian Insufficiency (POI)
Sometimes a woman’s ovaries can stop working normally before the typical age of menopause—usually before 40. This is called premature ovarian insufficiency (POI), and it’s often linked to autoimmune disorders, chemotherapy, or genetic factors. Because ovarian dysfunction affects reproduction, some symptoms can look a lot like PCOS.
The key difference? With PCOS, menstrual and reproductive issues usually start around puberty. If your reproductive symptoms appear later in your 30s, POI is more likely. POI also rarely affects male sex hormones, so signs of high androgens (like excess hair growth or acne) aren’t usually part of the picture.
Overlapping Symptoms of PCOS and Premature Ovarian Insufficiency:
- Irregular or absent periods
- Infertility
- Depression and mood swings
- Fatigue
- Scalp hair thinning
- Sleep disturbances
Distinct Symptoms of Premature Ovarian Insufficiency:
- Hot flashes and night sweats
- Vaginal dryness
- Low bone density
- Low libido
Metabolic and Lifestyle-Related Issues
We’ve talked a lot about how hormonal imbalances are a core issue of PCOS, causing symptoms that overlap with many conditions. But there’s another root problem: insulin resistance. Up to 80% of women with PCOS have this metabolic issue, so it’s super common among Cysters.
Insulin resistance occurs when your body doesn’t convert glucose into energy properly. Instead, glucose stays in the bloodstream and gets stored as fat. This can lead to substantial metabolic dysfunction, which is why PCOS can sometimes be confused with other metabolic conditions.
Metabolic Syndrome
This one is particularly confusing because you can have metabolic syndrome with PCOS. That said, you can also have metabolic syndrome without PCOS. Metabolic syndrome is a cluster of conditions that affect your cardiovascular and metabolic systems. If a person has three of the following problems, they have metabolic syndrome:
- Obesity
- High blood pressure
- Insulin resistance
- Bad cholesterol.
All of those are indeed possible with PCOS as a result of insulin resistance. The important thing to note is that metabolic syndrome won’t involve significant hormonal symptoms. So, if you have metabolic side effects, but no hormonal ones, you may have metabolic syndrome and not PCOS. On the other hand, if you’re experiencing side effects of each together, you could be dealing with both conditions.
Overlapping Symptoms of PCOS and Metabolic Syndrome:
- Weight gain, especially around the abdomen
- Insulin resistance/high blood sugar
- Fatigue
- Irregular cholesterol levels (low HDL, high triglycerides)
- High blood pressure
Obesity-Related Issues
Obesity can cause a lot of problems in the body—and a lot of those issues look like PCOS! It can actually trigger all three of PCOS’s root issues: hormonal imbalance, inflammation, and insulin resistance.
Extra fat tissue reduces insulin sensitivity and prompts the body to produce more estrogen, resulting in both hormonal and metabolic symptoms. It can also contribute to chronic, low-grade inflammation, triggering digestive issues, body pain, skin problems, and brain fog. In comparison, all of these symptoms are also common with PCOS.
Though obesity-related issues and PCOS can be similar, there are distinct hormonal issues with PCOS not present in obesity alone. Namely, androgen levels aren’t elevated with obesity, and ovaries are usually unaffected (no cysts). So, if you’re experiencing symptoms of high male sex hormones or polycystic ovaries, you could have PCOS that’s just exacerbated by obesity.
Overlapping Symptoms of PCOS and Obesity-Related Issues:
- Weight gain
- Fatigue
- Depression and mood swings
- Irregular menstrual cycles
- Sleep problems
- Acne
- Darkened skin patches
- Brain fog
- Digestive issues
- Joint or muscle aches
Distinct Symptoms of Premature Obesity-Related Issues:
- Shortness of breath
- Fatty liver disease
- Gallstones
- Pressure sores
- Slow wound healing
Type 2 Diabetes
As I’ve said, insulin resistance is a big problem with PCOS. And you know the primary disorder associated with poor insulin processing, right? It’s type 2 diabetes. When you have type 2 diabetes, your body can’t use insulin effectively. This inevitably leads to high insulin resistance and all the symptoms that come with it.
Like the other metabolic issues we’ve talked about, women with PCOS often have type 2 diabetes as well. In fact, they’re at 8 times greater risk of developing type 2 diabetes due to unchecked insulin resistance.
However, there are times doctors may think you have type 2 diabetes when you’re actually dealing with PCOS—or both conditions together! Type 2 diabetes is not hormonal, so hormonal symptoms aren’t common with T2D alone. Additionally, thyroid and sex hormone levels remain normal—the problems all center on metabolism.
Overlapping Symptoms of PCOS and Type 2 Diabetes:
- Weight gain
- Fatigue
- Depression and mood swings
- Darkened skin patches
- Brain fog
- Sleep disturbances
- Digestive issues or bloating
Distinct Symptoms of Type 2 Diabetes:
- Increased thirst and frequent urination
- Slow wound healing
- Numbness or tingling in hands or feet
- Blurred vision
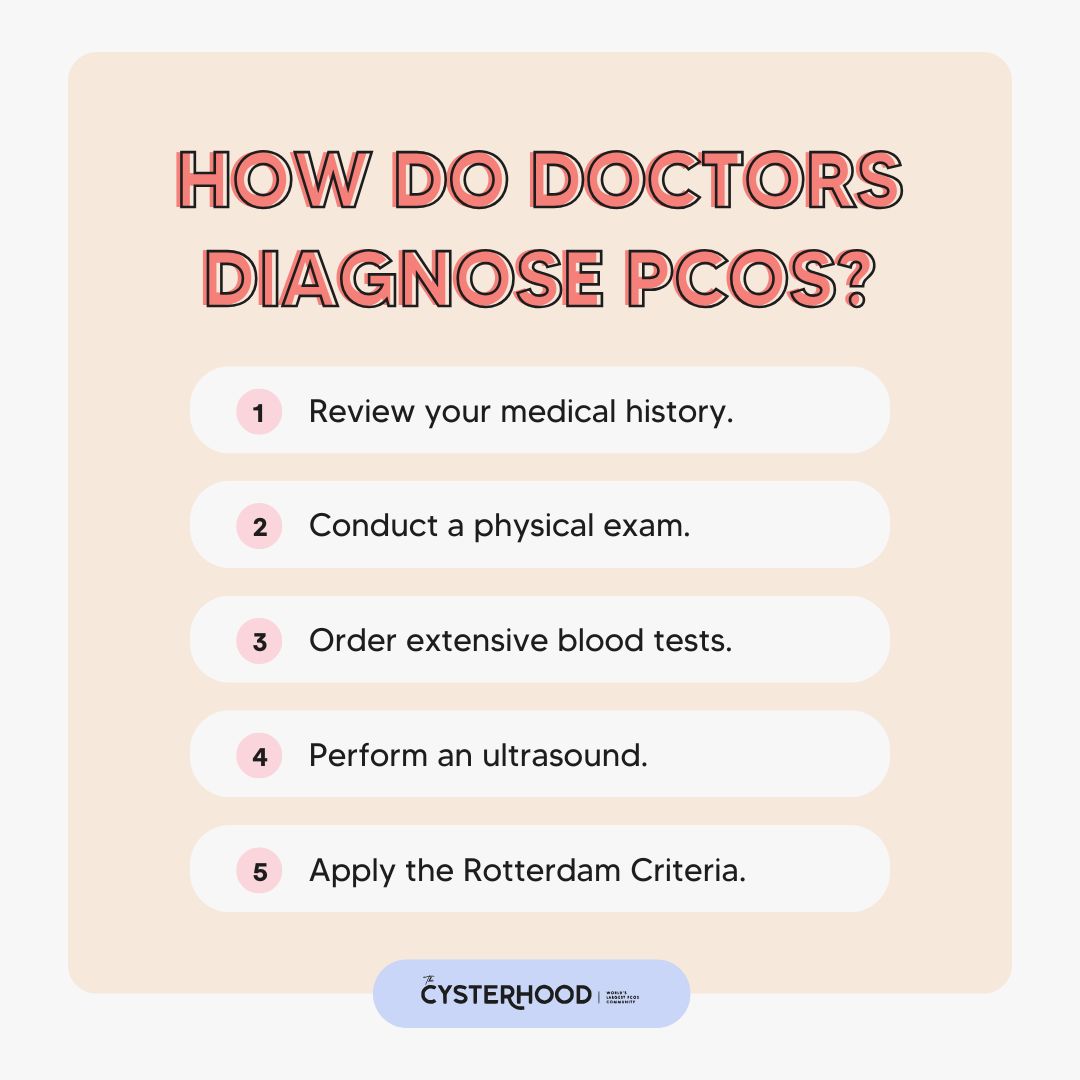
How Do Doctors Diagnose PCOS?
Step 1: Review your medical history.
First, your doctor will review your medical history, including family history, current symptoms, existing conditions, medications, and lifestyle factors.
Step 2: Conduct a physical exam.
Next, the doctor will do a physical exam to look for visual signs of PCOS. Physical signs of PCOS include excess body and facial hair, scalp hair loss, acne, high body weight, and dark skin patches, to name a few.
Step 3: Order extensive blood tests.
To definitively diagnose PCOS, you need a blood test. However, ensure your doctor does a pretty thorough one. Not all of them are sensitive enough to detect insulin and hormone levels common with PCOS. I recommend this blood test from EquiLife if you decide to go private.
Step 4: Perform an ultrasound.
Many Cysters have polycystic ovaries, even if they’re asymptomatic. Fortunately, though, pelvic ultrasound can identify ovarian cysts. As a result, this rules out a lot of other potential conditions, helping doctors be confident in their PCOS diagnosis.
Step 5: Apply the Rotterdam Criteria.
The Rotterdam Criteria are a set of key features in PCOS. If you have at least 2 of the 3, you can be diagnosed with PCOS after other conditions have been ruled out. Here are the criteria:
- Irregular or Absent Ovulation
- High Androgen Levels
- Polycystic Ovaries
Consider: Diagnosis May Not Be Clear
Understand that diagnosing PCOS can be really difficult. If you think you have PCOS, but the doctor is unsure, keep advocating for yourself, consider seeing a different provider, and get a head start on your healing. Download The Cysterhood app and read my essential guide to managing PCOS naturally to take your health into your own hands.

Why Is It Important to Get the Correct Diagnosis for PCOS?
To find relief, you need to know what your core issues are. The wrong diagnosis can mean wasting lots of time, money, and effort on treatments that don’t improve quality of life. When you have the right diagnosis, you can be confident that every lifestyle change and medical action is one step closer to symptom relief and true healing!
Many conditions can be mistaken for PCOS; be confident you have an accurate diagnosis.
PCOS comes with a bunch of symptoms, and a lot of them overlap with other conditions. Knowing what’s shared and what’s unique can help you get the right diagnosis. From there, you can focus on the root cause, skip treatments that don’t work, and actually manage your symptoms long-term. Staying informed and speaking up for yourself makes a huge difference!
For more, make sure you browse the PCOS Weight Loss blog and listen weekly to A Cyster and Her Mister Podcast. I can’t wait to be a part of your healing journey!







