PCOS stands for Polycystic Ovary Syndrome—but if we’re being honest, the name is pretty unhelpful. It doesn’t tell the full story, and it definitely doesn’t reflect what most of us actually experience with PCOS.
That’s a problem, because a vague (and honestly, a bit misleading) name can make it harder for women to get an accurate diagnosis or truly understand what’s going on in their bodies.
So in this post, I want to give you a clear, comprehensive overview of polycystic ovary syndrome (PCOS). I’ll break down what PCOS really is, how it affects the body, and the different ways it’s treated. When you understand what’s actually driving your symptoms, healing and finding real relief feel much more attainable.
Here’s what you need to know about PCOS:
What Does PCOS Stand For? Understanding the Condition
Okay, let’s break down the name:
- POLYCYSTIC
- OVARY/OVARIAN
- SYNDROME
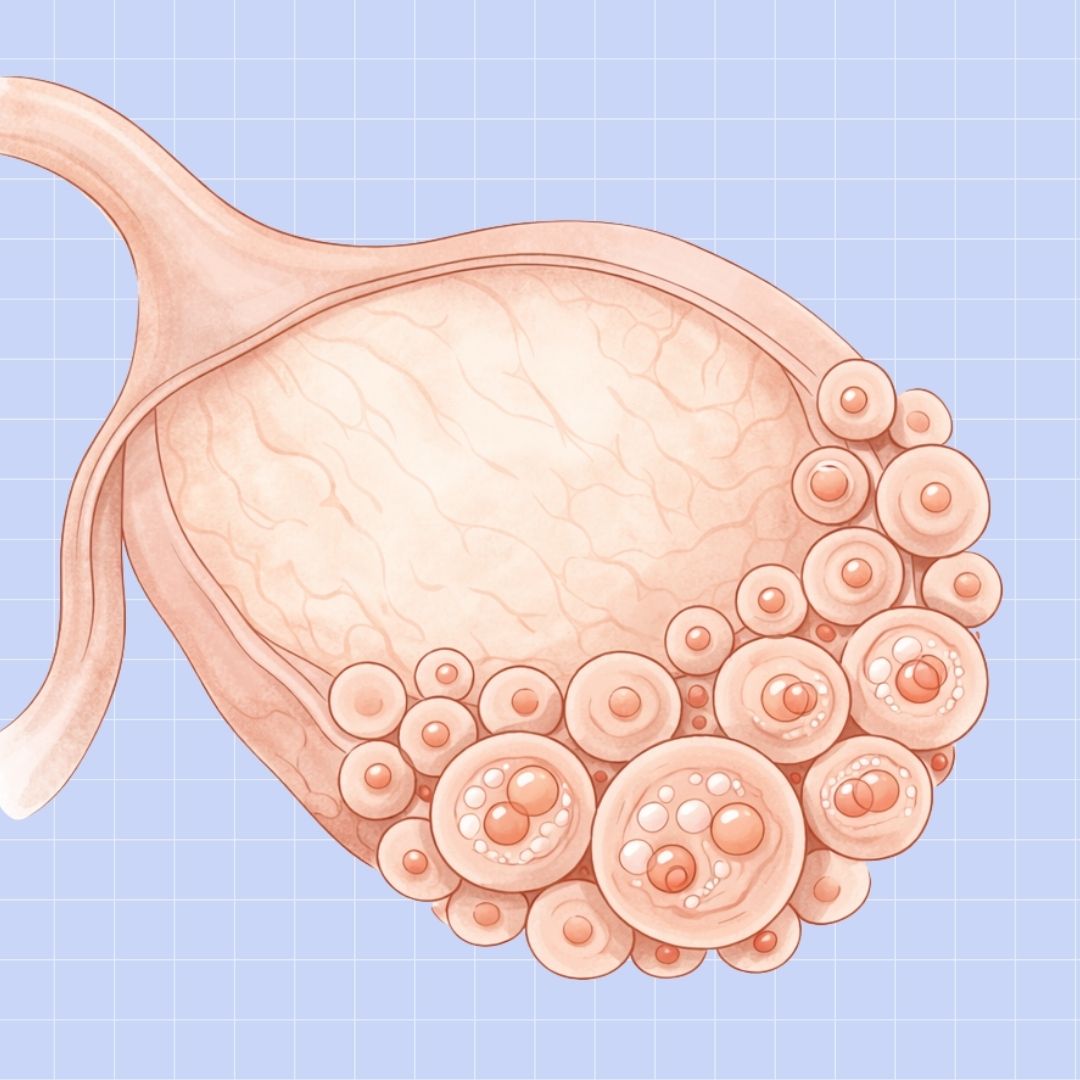
The name Polycystic Ovary Syndrome refers to the polycystic appearance sometimes seen in the ovaries of women with PCOS. Because of elevated androgen levels, the ovaries may produce many immature follicles rather than a single dominant, viable egg. Over time, those underdeveloped follicles can accumulate, creating the classic “string of pearls” appearance seen on ultrasound.
Here’s the problem: around 40% of women with PCOS do not have polycystic ovaries at all. And even among those who do, this feature is rarely the most disruptive or challenging part of living with PCOS day to day.
The name itself comes from what doctors first observed about the condition nearly a century ago. In 1935, Irving F. Stein and Michael L. Leventhal published a paper describing women with enlarged ovaries filled with fluid-filled follicles, along with irregular periods and infertility. They originally called it Stein–Leventhal syndrome, which was later renamed Polycystic Ovary Syndrome sometime in the 60s.
Unfortunately, the name stuck… even as research expanded and our understanding of PCOS evolved. Today, we know PCOS involves far more than irregular periods and ovarian appearance. It’s a complex hormonal and metabolic condition that affects the entire body, not just the ovaries.
What Causes PCOS?
The cause of PCOS is unknown. We do know what drives the symptoms of PCOS, but there’s no definitive trigger that sets everything into motion (that we know of).
PCOS does seem to run in families, but there isn’t a single PCOS gene. Instead, multiple genes appear to contribute to things like chronic inflammation, insulin resistance, and hormone imbalances. These core issues ultimately cause the PCOS symptoms listed below.
What Are the Signs and Symptoms of PCOS?
Metabolic and Blood Sugar Symptoms
- Insulin resistance
- Sugar or carbohydrate cravings
- Difficulty losing weight
- Stubborn weight gain (especially around the abdomen)
Digestive and Inflammatory Symptoms
- Bloating
- Digestive discomfort
- Puffiness or fluid retention
- Joint or muscle aches
Energy, Mood, and Mental Health Symptoms
- Anxiety or depression
- Chronic fatigue
- Brain fog
- Mood swings
You can learn more about this connection in my post, “PCOS and Mental Health.”
Reproductive and Fertility Symptoms
- Missed or irregular periods
- Very heavy or very light periods
- Difficulty getting pregnant
- Irregular or delayed ovulation
- Poor egg quality
- Thickened uterine lining
- Reduced cervical mucus
- Recurrent miscarriage
Skin and Hair Symptoms
- Excess facial or body hair (hirsutism)
- Thinning scalp hair or hair loss
- Persistent adult acne
- Oily skin or scalp
- Darkened skin patches (acanthosis nigricans)
- Skin tags
Can You Have PCOS Without Symptoms?
Technically, yes. However, without the trademark signs of PCOS, it would be next to impossible to know you have the condition. For most Cysters, it takes years to get a diagnosis. Running all the tests, assessing symptoms, and ruling out other health problems takes a long time. If you’re asymptomatic, doctors probably wouldn’t even be willing to entertain the idea that you have PCOS.
If you think you have PCOS but consider yourself asymptomatic, I’d encourage you to look again at the list of symptoms above. You may have some of the issues listed but simply didn’t realize they could be part of PCOS or connected to other chronic problems. Many PCOS symptoms are subtle, internal, or easy to normalize—especially when they’ve been present for years.
If you want a deeper exploration into this conversation, visit: “How to Know If You Have PCOS: A Guide to Symptoms and Testing.”
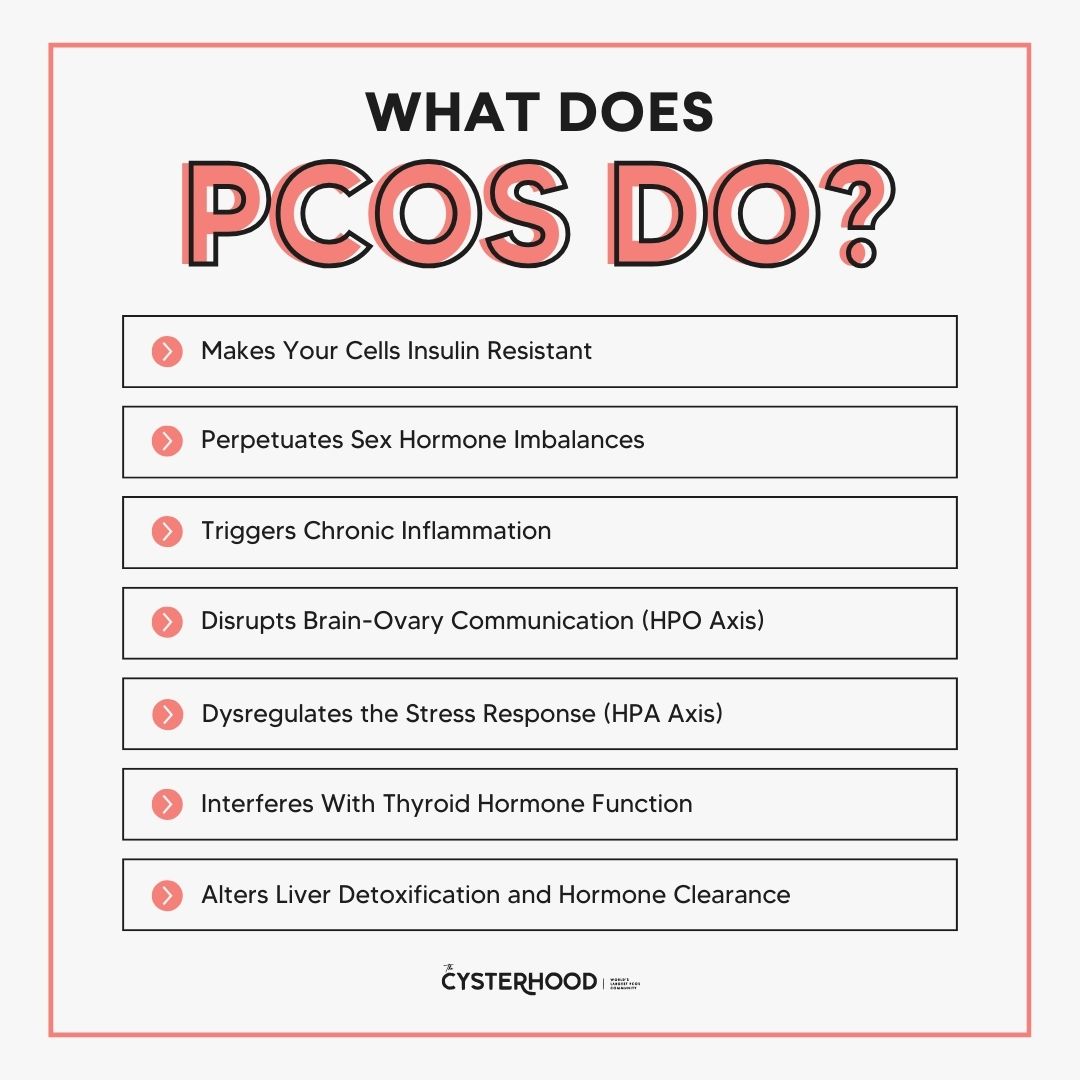
What Does PCOS Do?
As I mentioned earlier, PCOS doesn’t have a known cause. That said, we do understand how it affects the body and where PCOS symptoms come from. You can trace most of your symptoms back to one or more of the root issues below.
You may not experience all these core problems, depending on your PCOS type. But remember, this condition exists on a spectrum. That means some women deal with more dysfunction than others. Still, these are the most common underlying issues women with PCOS face:
Makes Your Cells Insulin Resistant
PCOS often prevents cells from responding properly to insulin. Instead of efficiently turning sugar from food into energy, the body is more likely to store it as fat or leave excess glucose circulating in the bloodstream.
This leads to unstable blood sugar, elevated insulin levels, weight gain, and widespread metabolic dysfunction. Over time, insulin resistance can also put you at higher risk for type 2 diabetes, high blood pressure, and cardiovascular disease.
For more information, listen to this episode of my podcast on insulin resistance symptoms and natural treatment options.
Perpetuates Sex Hormone Imbalances
PCOS is both metabolic and hormonal. Imbalances in key sex hormones like estrogen, progesterone, luteinizing hormone (LH), follicle-stimulating hormone (FSH), and androgens drive many PCOS symptoms. This includes excessive hair growth, acne, irregular periods, mood issues, and infertility.
Triggers Chronic Inflammation
Many Cysters experience low-grade, chronic inflammation. This occurs when the immune system’s inflammatory response stays active long after a threat, like illness or injury, has passed. Ongoing inflammation damages tissues, disrupts normal bodily function, and worsens hormone imbalance, insulin resistance, and persistent fatigue.
Disrupts Brain-Ovary Communication (HPO Axis)
PCOS often disrupts communication between the brain and ovaries. Dysfunction in the hypothalamic-pituitary-ovarian (HPO) axis causes the brain to send mixed or mistimed signals to the ovaries.
This can lead to elevated luteinizing hormone, suppressed follicle-stimulating hormone, and further hormonal irregularities. As a result, ovulation may become inconsistent or absent even when periods appear regular.
Dysregulates the Stress Response (HPA Axis)
I just talked about the HPO axis, but now let’s talk about the HPA axis. In women with PCOS, there is often a disruption in the hypothalamic-pituitary-adrenal axis, which controls communication between the brain and the adrenal system.
This can lead to a heightened or poorly regulated stress response, causing cortisol levels to remain elevated or unstable. Over time, this worsens insulin resistance, fuels inflammation, and further disrupts hormone balance, making stress a major driver of PCOS symptoms.
Interferes With Thyroid Hormone Function
PCOS can cause altered thyroid hormone activity as well. Insulin resistance and chronic inflammation can interfere with the body’s ability to properly convert thyroid hormone into its active form at the cellular level. When this conversion is impaired, metabolism can slow, and hormone clearance becomes less efficient. This contributes to fatigue, weight struggles, and persistent hormone imbalances often seen with PCOS.
Here’s more on PCOS and thyroid dysfunction.
Alters Liver Detoxification and Hormone Clearance
The liver plays a critical role in clearing excess hormones from the body. In PCOS, however, insulin resistance and inflammation can impair liver detoxification pathways, resulting in reduced clearance of adrenal metabolites. This prevents your body from fixing the many hormone imbalances you’re dealing with.

How Is PCOS Diagnosed?
Step 1: Medical History and Symptoms Review
First, your doctor will review your full medical history. This includes existing health conditions, current medications, past hospitalizations, family health history, prior lab work or imaging, and lifestyle factors. The goal is to identify patterns that align with a PCOS diagnosis and rule out other conditions that may cause similar symptoms.
Which, if you’re interested in learning about, are covered in my post: “What Can Be Mistaken for PCOS? Conditions with Similar Symptoms.”
Step 2: Physical Examination
Next, you’ll have some kind of physical exam. Don’t worry, this isn’t usually too invasive. Your provider will check basics like height, weight, and blood pressure. They’ll also check your body fat distribution, since many women with PCOS carry more weight in the abdominal area.
They may examine your skin and hair for signs of hormone imbalance, like acne or excess hair growth. Your doctor might also check your neck for thyroid enlargement, and in some cases, perform a pelvic exam depending on the type of provider you’re seeing and the care you’re seeking.
Step 3: Extensive Blood Testing
Blood testing is another big part of diagnosing PCOS. And here’s the thing: there’s no single key measurement that conclusively indicates whether you have the condition. Instead, doctors will look for hormone patterns and metabolic disruptions. Here are some labs they’ll likely order (again, depending on the type of healthcare provider):
- Reproductive and Androgen Hormone Testing
- Glucose and Insulin Metabolism Markers
- Thyroid Function Tests
- Lipid Panel (Cholesterol and Triglycerides)
- Inflammatory Markers
- Adrenal and Cortisol Testing
Step 4: Ultrasound
Many doctors will also perform an ultrasound to look for that trademark “polycystic” look to the ovaries. Yes, not every woman with PCOS has this symptom. Still, if it is visually obvious on the ultrasound, it can fast-track you to a diagnosis.
Step 5: Diagnostic Criteria Assessment
Finally, your doctor will apply the Rotterdam criteria. This guideline states that doctors can diagnose PCOS if two of the following three factors are present:
- Polycystic ovaries
- Irregular periods or ovulation
- High androgen levels
Even then, it’s possible not to get a clear diagnosis right away. PCOS can be tricky, and providers who aren’t deeply familiar with its hormonal and metabolic nuances may miss the bigger picture. So if one practitioner rules it out but your symptoms persist, that doesn’t necessarily mean PCOS is completely off the table.
How Is PCOS Treated?
There is no single cure for PCOS. However, there are a lot of ways you can manage your condition and find relief! Here’s what you can do:
Lifestyle-Based Treatment (Root-Cause Support)
Here at PCOS Weight Loss, I am all about naturally reversing your PCOS through intentional lifestyle changes. By getting to the root issues of insulin resistance, hormonal imbalance, and chronic inflammation, you can lose weight, regulate your periods, and live symptom-free with PCOS.
And you don’t have to do it alone. Download The Cysterhood app, where you can find recipes, workouts, and a community here to support you. You can also read my guide, “How to Manage PCOS Symptoms Naturally,” for a head start.
Medication-Based Treatment (Symptom Management)
You’ll find providers who aren’t well-versed in PCOS usually jump to prescription drugs to help manage PCOS. This can be effective for masking symptoms, but it doesn’t fix the root issues. Meaning, as soon as you get off the meds, your symptoms return. Plus, most medications have side effects that can just add to your list of chronic symptoms!
That said, I understand every situation is different. For some women, a mixture of lifestyle-based treatments and supportive medications can be really effective. If hormone balance is the primary concern, providers may prescribe hormonal birth control pills or anti-androgen drugs like spironolactone. And if improving metabolic health is the goal, they may offer GLP-1 medications or Metformin.
It’s best to do your own research and get second opinions before starting any prescriptions to manage PCOS.
Fertility-Focused Treatment
If getting pregnant is your main goal, treatment for PCOS may look a little different. Fertility-focused care is designed to support regular ovulation, improve egg quality, and strengthen the hormonal environment needed for pregnancy. This can include targeted lifestyle changes, cycle-supportive supplements, and medications that stimulate ovulation.
In some cases, providers may also prescribe progesterone support (like progesterone shots, suppositories, or oral progesterone) after ovulation or during early pregnancy. This helps support the uterine lining and reduce the risk of early pregnancy loss, which can be more common in women with PCOS.
The focus here isn’t just conceiving. It’s creating a hormonal and metabolic environment that can actually sustain a healthy pregnancy. For a deeper conversation about pregnancy and PCOS, read my post: “Can You Develop PCOS After Pregnancy?”
Symptom-Specific Treatment
Some women choose to focus on managing their most disruptive symptoms first. Symptom-specific treatment targets things like acne, excess hair growth, hair thinning, irregular periods, or fatigue. Addressing these problems may involve a mix of nutrition strategies, supplements, topical treatments, and medications, depending on what you’re trying to fix.
While this approach can bring some relief, it works best when paired with root-cause support to prevent symptoms from cycling back. Plus, when you address core issues, you can improve multiple side effects at once.
Remember: this doesn’t have to be an isolating experience. Visit my essential guide to managing PCOS naturally for a deeper, more comprehensive overview.
PCOS is much bigger than polycystic ovaries and irregular periods.
PCOS is a complex hormonal and metabolic condition that affects the entire body, which is why it can look so different from one woman to the next. When you understand what is actually driving your symptoms, PCOS becomes far less confusing and much more manageable.
With the right information, support, and approach, real healing is totally possible. For more resources, join the Cysterhood, browse the rest of the blog, and listen regularly to A Cyster and Her Mister wherever you listen to podcasts! We’re here to help.