Polycystic ovarian syndrome (PCOS) is a metabolic disorder that affects women of reproductive age and is characterized by hormonal imbalances. These hormonal imbalances affect many parts of the body, including the reproductive system.
With reproductive system problems, many Cysters face issues with menstrual cycles and fertility. When a Cyster does become pregnant, unfortunately those pregnancies are much more likely to end in miscarriage and pregnancy loss compared to pregnancies of women without PCOS.
Today, I’m dedicating this post to PCOS and pregnancy loss. I’ll discuss how they could be related and how you can go about reducing miscarriage risk. As always, there is still plenty of hope for a viable pregnancy!

PCOS and Miscarriage
Miscarriage is a sudden pregnancy loss usually within the first 20 weeks. In this post, we’ll also discuss late-term pregnancy loss as well. The rate of miscarriage in women without PCOS is between 10%-15% of pregnancies. But, for Cysters, the miscarriage rate increases to a heartbreaking 30%-50%.
This seems to suggest a link between PCOS and miscarriage. You can learn more about how pregnancy affects PCOS here. Below, I’ll dive more into how PCOS and miscarriage are related!
Does PCOS Cause Miscarriage?
Research suggests polycystic ovary syndrome (PCOS) increases the risk of miscarriage. However, the exact reason for the heightened risk isn’t super clear. Studies suggest 3 possible associations.
Hormonal Imbalances
PCOS is a hormonal condition, so imbalances of important reproductive hormones are a common cause of miscarriage and infertility. A healthy pregnancy requires your body to have optimal balance of important hormones for successful implantation and pregnancy development.
So, what hormonal imbalances could specifically lead to miscarriage? Here’s what to look out for:
Low Progesterone
Cysters often have irregular periods. In fact, it’s one of the three main PCOS diagnostic criteria. Skipping a period might not seem like a big deal, and sometimes it even feels like a relief, but it can set off a domino effect when it comes to fertility.
When we do not ovulate or ovulate poorly, the ovaries do not produce enough progesterone. Progesterone is what prepares the uterus for a baby and helps maintain a healthy uterine lining. If the lining is not ready, a fertilized egg may struggle to implant properly, increasing the risk of miscarriage. Low progesterone is actually a common cause of recurrent pregnancy loss.
High Estrogen
Progesterone is produced during the menstrual cycle to balance estrogen. Estrogen is responsible for building up the uterine lining throughout the cycle. When progesterone is released during the luteal phase, it stops the build-up at just the right time, making the lining receptive enough for implantation but strong enough to hold the embryo in place. Once pregnancy begins, progesterone takes over to maintain the uterine lining for the entire pregnancy.
When progesterone is too low, there is nothing to balance the estrogen, so the lining keeps building until it becomes thick and unstable, which is not ideal for an embryo. This is why periods can be especially painful for women with PCOS, because there is extra lining to shed. Even if an embryo attaches to the uterine wall, if there is not enough progesterone to maintain the lining, it may eventually collapse, leading to miscarriage.
High Androgens
High androgens, like testosterone, are another common hormonal imbalance in women with PCOS. These are male sex hormones, and while some are necessary for overall hormone balance, too much can disrupt the female reproductive system.
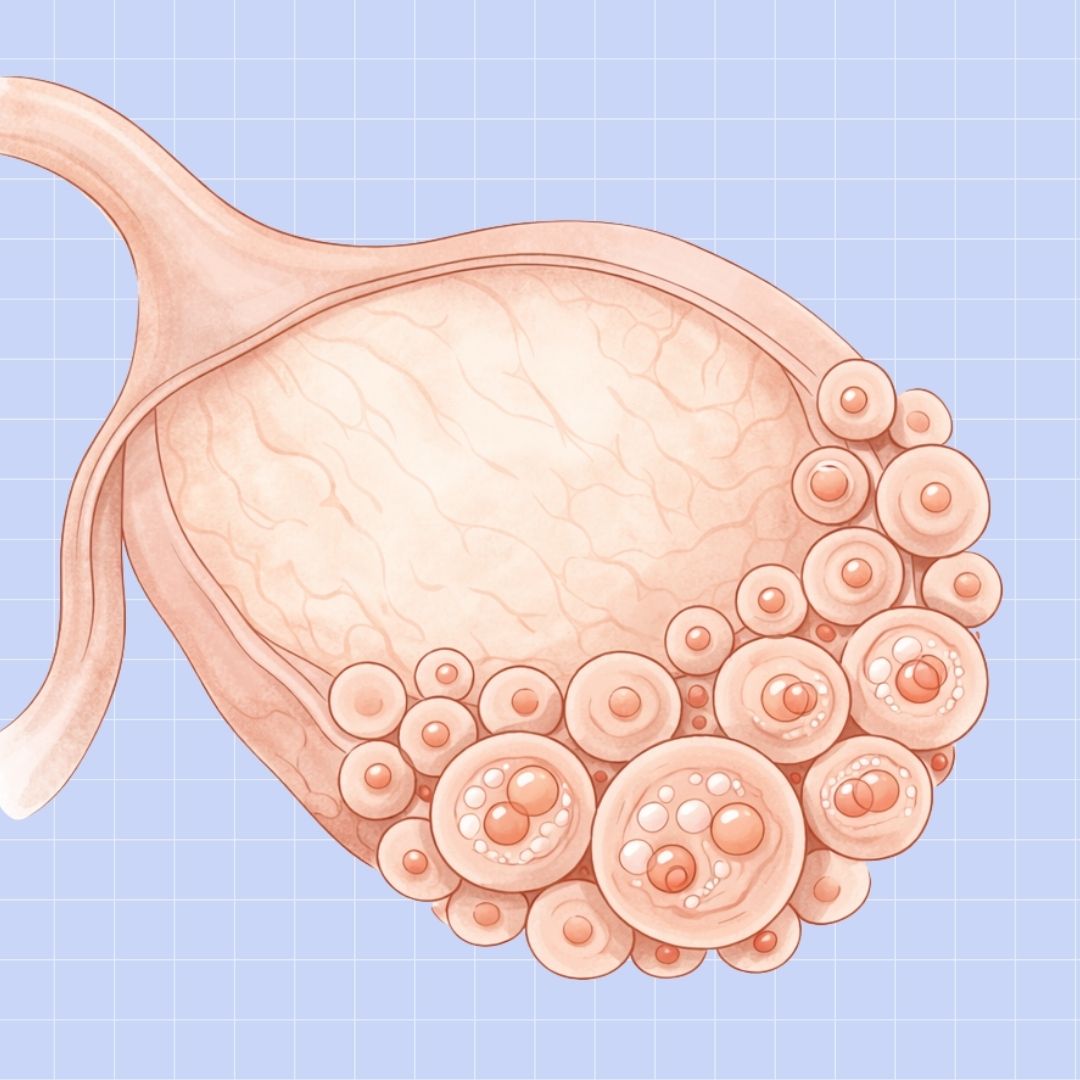
When androgen levels are high, they interfere with the development of follicles, or eggs. Instead of one mature follicle forming, many small, immature follicles develop. This is where the term “polycystic” comes from. As a result, either no egg is released at all, leading to cysts, or the egg that is released may have abnormalities, making it less viable and increasing the risk of miscarriage.
High Luteinizing Hormone
Women with PCOS often have excess LH, or luteinizing hormone, due to a miscommunication between the brain and the pituitary gland. LH helps regulate ovulation, so when it stays high, it disrupts normal follicle growth, leading to premature ovulation or no ovulation at all. High LH also stimulates the body to produce more androgens, which, as we’ve discussed, can harm egg quality and ovulation.
When a Cyster’s body has too much LH, it is not fully prepared to support pregnancy. The eggs may be abnormal, the uterine lining may be unstable, and hormones needed for fetal development may be out of balance, all of which can increase the risk of miscarriage.
Insulin Resistance and Inflammation
A systematic review of PCOS patients found that up to 80% of Cysters have insulin resistance. This happens when cells do not convert glucose into energy properly, leaving it in the bloodstream and storing it as fat. This raises body weight and blood sugar levels. High insulin levels can then trigger the ovaries to produce more androgens, which, as we’ve discussed, negatively affects egg quality and ovulation.
Insulin resistance also signals the body that it is under stress, which triggers inflammation. Chronic, low-grade inflammation increases oxidative stress and can damage the embryo early on, interfering with placental development. In severe cases, inflammation may even prompt the immune system to attack the embryo, leading to miscarriage.
Consistently high blood sugar also increases the risk of Gestational Diabetes Mellitus (GDM), a type of diabetes that occurs during pregnancy. Numerous studies, including this recent meta-analysis, find that GDM can affect embryo and placental development and is an independent risk factor for miscarriage, especially in the first trimester.
High Body Weight and Metabolic Issues
Insulin resistance and hormonal imbalances can contribute to high body weight and other metabolic issues, such as high blood pressure, high blood sugar, and high cholesterol. This combination of problems can significantly increase miscarriage risk because it can cause many of the issues we’ve already discussed: an unstable uterine lining, poor egg quality, gestational diabetes, embryo damage, impaired placental development, and immune system attacks on the embryo.
High body weight also raises the risk of microvascular dysfunction and hypercoagulability, which are just fancy ways of saying the body is more likely to form blood clots. These microclots can develop in the placenta, reducing oxygen and nutrient supply to the baby and increasing the chances of miscarriage.

PCOS Miscarriage Rates and Statistics
- A Cyster is 3 times more likely to experience early pregnancy loss than a woman without PCOS. (source)
- 5.4% of PCOS pregnancies end in third-trimester loss, whereas only 3.1% of non-PCOS pregnancies have the same conclusion. (source)
- Maternal age and BMI have a great effect on increasing miscarriage rates over PCOS alone. (source)
- IVF (in-vitro fertilization) and intrauterine insemination (IUI) pregnancies are 2 times more likely to result in miscarriage. (source)
- 40%-80% of women with recurrent miscarriages have PCOS. (source)
- Pregnant women with PCOS are 9 times more likely to develop gestational diabetes than a pregnant woman without PCOS. (source)
Can Miscarriage Cause PCOS?
No. PCOS can increase the risk of miscarriage, but miscarriage does not cause PCOS. Neither pregnancy nor miscarriage causes long-term hormonal or metabolic problems. You might feel like your hormones are out of balance for a while afterward, but once your body has fully healed, things usually return to normal.
If you notice PCOS-like symptoms after a miscarriage, it is worth talking to your doctor. Miscarriage can cause dramatic shifts in estrogen, progesterone, and LH, so irregular cycles or other symptoms are normal at first. After a few cycles, your hormones should stabilize.
If your period has not returned, call your doctor right away. This could indicate retained tissue from the pregnancy. A simple hCG test can confirm that everything is clearing properly. Additionally, there’s also something called post-miscarriage infection. It’s rare, but it’s essentially uterine inflammation that can interfere with ovarian function and make periods irregular. Either way, you need to confirm there’s no lasting problems!
Sometimes PCOS-like symptoms after miscarriage are related to thyroid problems. Miscarriage can reveal thyroid disorders, particularly subclinical hypothyroidism. The miscarriage itself does not cause the thyroid problem, but the extra demands on the thyroid during pregnancy can make previously hidden issues apparent.
Symptoms of subclinical hypothyroidism include fatigue, weight gain, hair loss, mood swings, swelling, irregular periods, and fertility difficulties. If you experience persistent problems after miscarriage, talk to your doctor about lab tests to check thyroid and prolactin function.
Can IVF Decrease the Chance of Miscarriage in PCOS?
Assisted reproductive technologies like IVF, frozen embryo transfer, or intracytoplasmic sperm injection (ICSI) can improve your chances of conception. However, they do not automatically guarantee a healthy pregnancy outcome in PCOS. If insulin resistance, inflammation, hormonal imbalances, or other underlying issues are not addressed, the risk of miscarriage could be just as high.
But don’t worry. These conditions are totally reversible! Follow the lifestyle changes below to heal your PCOS for you and your future baby.

How To Avoid Miscarriage With PCOS
Exercise regularly.
Exercise can have many PCOS benefits! First of all, regular exercise can help you maintain a healthy weight. Since a high BMI can significantly increase the risks of miscarriage, pregnancy complications, and gestational diabetes, getting to a healthy weight should be a priority. (Easier said than done, I know. Here’s more on how to lose weight with PCOS.)
Beyond helping you lose weight, exercise can also help you reduce stress, lower blood glucose levels, and balance hormone levels—these all have a positive impact on pregnancy. However, I don’t recommend all kinds of exercises. Here are the workouts I’ve found are most beneficial for PCOS.
Eat the right foods.
A balanced diet is another good way to lose weight, balance hormones, and have a healthier pregnancy. As a nutritionist who specializes in PCOS, I recommend an anti-inflammatory gluten- and dairy-free diet. The diet isn’t just about what not to eat, it’s also about what PCOS-fighting foods you should eat.
When you download The Cysterhood app, you’ll find delicious PCOS-friendly meals and exercise plans that’ll help you lose weight and reverse the effects of PCOS. As your body regulates and gets back to a healthy state, pregnancy viability will hopefully improve as well! Here’s more on how to heal from PCOS using this diet.

Take the right supplements and vitamins.
Even with a well-balanced diet, getting all the nutrients your body needs to thrive is really hard. Nutrient deficiencies can be a big contributor to hormone imbalance, insulin resistance, weight gain, and other symptoms negatively affecting your pregnancy outcomes.
First, talk to your doctor about getting a prenatal vitamin. Then, discuss other supplements like Ovasitol, vitamin D3, magnesium, omega-3, zinc, and CoQ10. Here’s more on my top recommended supplements for PCOS!

Reduce insulin resistance and blood sugar levels.
Insulin resistance is one of the main contributors to weight gain. If you have the insulin-resistant type of PCOS, your body doesn’t process sugar properly. Instead of the glucose being transformed into energy, it’s absorbed. It raises your blood sugar levels and causes weight gain, making getting to a healthy weight really difficult.
Insulin resistance also increases your chance of developing type 2 diabetes and gestational diabetes. Both are a concern for pregnancy viability. Luckily, the tips I’ve already mentioned: the right exercise, diet, and supplements can help lower insulin resistance. For more on insulin resistance and PCOS, listen to this episode of my podcast “A Cyster and Her Mister.”
Reduce stress.
Stress can worsen insulin resistance and hormone imbalances. What a lot of women miss is that they can’t get control of their weight and hormones without first reducing stress. I know it’s hard, but finding ways to relax, invest in yourself, and practice self-care is important for your mental and physical health. This will help with other PCOS symptoms too!
Cut caffeine.
Drinking more than 200 mg of caffeine a day during pregnancy has been linked to pregnancy complications and miscarriage. Plus, caffeine can increase the release of cortisol (AKA stress hormones), cause adrenal fatigue, and worsen insulin resistance, leading to weight gain, fatigue, and anxiety.
You can learn more about caffeine and PCOS here.
Get a good night’s sleep.
Poor sleep can have a significant impact on your mental and physical health. Lack of sleep can cause high blood pressure, hormonal imbalances, stress, insulin resistance, and potentially pregnancy complications. This can be challenging since people with PCOS often struggle with sleep disorders like insomnia and sleep apnea. However, prioritizing getting better sleep can have big benefits for your health, which can help lower your risk of miscarriage.
Though there is an increased risk of miscarriage if you have PCOS, healthy pregnancies are possible!
Becoming a mother is something so many women with PCOS long for. However, infertility and miscarriage stemming from PCOS can make the process emotionally and physically painful. (Here’s more on overcoming miscarriages and infertility.) But, have hope! By taking control of your PCOS, you can help lower your risk of miscarriage and increase your chances of having a successful pregnancy. Learn more about how to reverse your PCOS naturally on the blog and my podcast. Good things are ahead!