Polycystic ovary syndrome (PCOS) is usually marked by three common root issues: hormonal imbalances, insulin resistance, and inflammation. Most people know all about the hormonal side of things, but the other two issues can be just as problematic. Insulin resistance, for example, is one of the main reasons why Cysters struggle to lose weight, constantly feel fatigued, develop skin tags, and are at an increased risk of type 2 diabetes and heart disease.
Insulin resistance is when your cells don’t respond properly to glucose. Instead of converting the sugar into energy like it’s supposed to, it’s absorbed into the bloodstream and stored in the body as fat. (Hello weight gain and high blood sugar levels!) Because of this issue, women with PCOS sometimes go hyperglycemic if the insulin resistance is not well-managed. This is when blood glucose is too high and can cause those long-term complications like diabetes.
But . . . what about hypoglycemia? Can women with PCOS experience low blood sugar as a result of their condition? That’s what we’re going to explore today!

What’s the Relationship Between PCOS and Hypoglycemia?
Women with PCOS actually CAN experience hypoglycemia. The specific type of hypoglycemia that Cysters should watch out for is reactive hypoglycemia. This is when your body produces an excessive amount of insulin while eating. This can sometimes happen when you eat meals with lots of carbs or you have insulin resistance or both!
Basically, all that excess insulin in your body post-meal causes your glucose levels to tank right after a meal. This may make you feel shaky, sweaty, dizzy, irritable, fatigued, and even hungry despite the heavy meal. It’s not normal to have these big fluctuations in fasting insulin levels, but it can happen if you have PCOS due to insulin resistance and hormonal imbalances that prevent insulin sensitivity and insulin stability.

Does PCOS Cause Hypoglycemia?
Usually, no. A Cyster is way more likely to experience hyperglycemia than hypoglycemia. However, the circumstances that can make your insulin levels way too high can actually make your insulin levels fall way too low too. The problem is with the body’s overproduction of insulin and your cell’s lack of response to insulin. It’s a bad combination that can have your blood sugar levels spiking and dropping all the time!
Not only can these peaks and valleys further increase your risk of long-term complications like heart disease and type 2 diabetes, but they can also cause a lot of unpleasant symptoms. Fatigue, headaches, brain fog, memory issues, and mood swings are all super common with women experiencing hypoglycemia or hyperglycemia.
How To Manage Hypoglycemia When You Have PCOS
Eat 3-4 balanced meals a day.
A good way to keep your blood sugar stabilized is to eat regular meals! I recommend 3-4 meals a day. Essentially, breakfast, lunch, and dinner with a snack in there somewhere. This will keep your blood sugar from dipping too low between eating times. Don’t skip meals!
If you’ve wondered about intermittent fasting, know that it still can work for someone with PCOS! I recommend fasting for no longer than 12 hours (most of that you’d be sleeping). For more on this, check out the episode of A Cyster and Her Mister about intermittent fasting and PCOS.
Opt for meals that are high in protein and healthy fats.
Protein and healthy fats are digested more slowly in the body. That means that carbs are absorbed slower too, which leads to a gradual release of glucose into the bloodstream. This can help prevent those spikes and dips! Because of the slower digestion, protein and healthy fats usually make you feel fuller longer, help you maintain energy levels, and actually help improve insulin sensitivity!
Be cautious of sugary foods and drinks.
I definitely am not here to say don’t eat any carbs. That’s just not sustainable! However, it’s a good idea to discover you carb tolerance and reduce your sugar intake.
If you want to learn how to discover your carb tolerance, or get ideas on how to get your sweet fix without compromising your health goals or you need more protein-rich meal ideas, download The Cysterhood app for all of my PCOS-friendly recipes and meal plans!
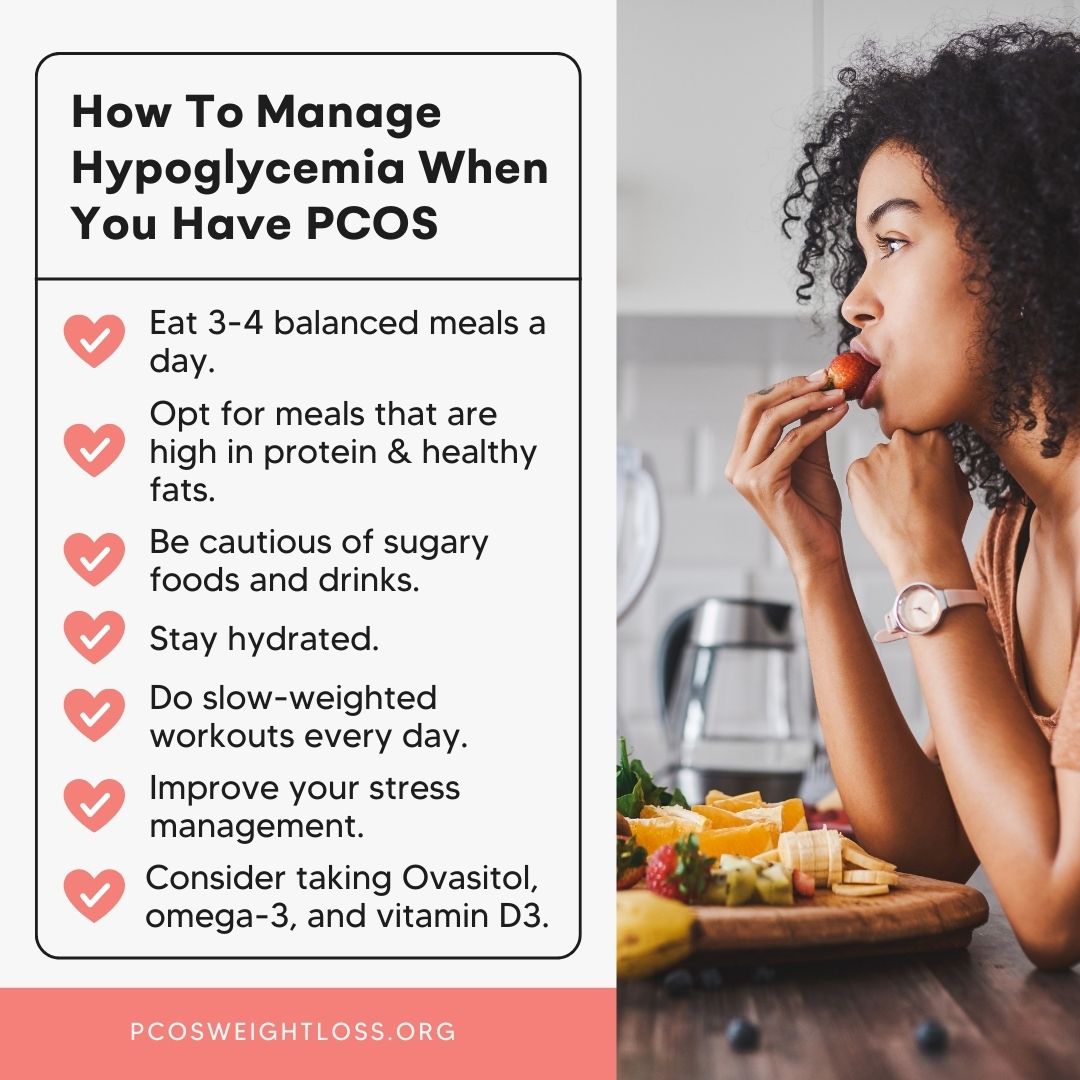
Stay hydrated.
Dehydration can worsen both hypoglycemia and hyperglycemia. Water is essential for diluting blood sugar in your bloodstream, supporting proper kidney function, balancing hormones, and increasing insulin sensitivity. Keep drinking water to keep your body in a healthy state.
Do slow, weighted workouts every day.
Exercise has been shown to help boost insulin sensitivity. Since insulin resistance is a main cause of hyperglycemia or hypoglycemia, regularly exercising is super important to prevent problems! However, you don’t want to do anything that increases your cortisol (stress levels), so slow-weighted or meditative workouts are best. You can find all the best PCOS-friendly workout routines on The Cysterhood app!
Improve your stress management.
Speaking of stress, it’s important to not only avoid increasing stress, but take steps to decrease it too. Stress actually worsens insulin resistance! So, practice self-care, get out in nature, start mediating whatever you need to keep those cortisol levels down.
Consider taking Ovasitol, omega-3, and vitamin D3.
Supplements can be a big help to support your body in proper blood sugar regulation! Studies show that Ovasitol, omega-3, and vitamin D3 can all improve insulin sensitivity. You can get all of those from Ovafit!

PCOS can lead to spikes and drops in blood sugar, but you can naturally regulate your levels!
Polycystic ovary syndrome (PCOS) can really impact your metabolic health. Insulin resistance is probably a cause of lots of your chronic symptoms! Luckily, you can naturally regulate your blood sugar levels and reverse your symptoms.
Find out more about naturally healing PCOS on the PCOS Weight Loss blog and the A Cyster and Her Mister podcast!